INTRODUCTION
Menisci help in shock absorption and load transmission, and assist in maintaining the integrity and nutrition of the chondral surfaces.1 Meniscal tears are some of the most common knee injuries and are secondary to some form of trauma. 2
Millions of arthroscopic surgeries for meniscal pathology are performed globally.3 Usual options include repair or debridement. Repair is generally preferred in younger patients to prevent increased loading through the affected compartment, leading to progressive degenerative change.4,5 Full vascularization of the meniscus happens shortly after birth. However, at maturity only the peripheral 10 – 25% retains blood supply, thus the meniscus is divided into a main outer vascular zone and an inner avascular zone, referred to as the red-red zone and white-white zones respectively, and these zones are further separated by the so-called red-white region. The healing capacity of each area is directly related to the vascularity and hence the injured area of the meniscus may heal or be permanently damaged depending on the zone of injury.6
There is still a debate onwhether meniscal repair or meniscectomy gives better results. Healing rates reported for repaired menisci are variable, with some literature suggesting that isolated meniscal repair without concomitant ACL reconstruction leads to low rates of healing and high rates of re-tear.7
Many techniques for meniscal repair have been described. Over the last 30 years, arthroscopic repair techniques have evolved significantly and become popular.8,9 An all-inside technique to repair meniscus has become popular over an outside-in technique, being considered less harmful to neurovascular structures.10,11 Haas et al. evaluated the FAST-FIX 360 suture device (Smith and Nephew, London, UK) for meniscal repairs and concluded that the success and complication rates were high and low respectively and gives results comparable to classic suture repair techniques.12 Meniscal repair with or without concomitant anterior cruciate ligament (ACL) repair has been found to have differing success rates, and ACL reconstruction was found to be protective for meniscal re-injury. Also, evidence suggests that isolated meniscal repair without ACL reconstruction is unreliable,13but this has not been confirmed.14
The aim of this study was to evaluate the clinical outcomes of meniscal repairs in our practice and perform an analysis of isolated vs concurrent ACL and meniscal repair.
MATERIALS AND METHODS
We identified and reviewed the records of a consecutive series of 53 patients with meniscal tears that underwent repair, over a two-year period. All the operations were performed by a single surgeon with post-graduate fellowship training in sports knee surgery, using a tourniquet and under general anaesthesia. Surgical reparability and absence of osteoarthritis were the determining factors leading to meniscal repair, independent of patient age or the vascularity zone as described above. Any meniscal tear not deemed to be repairable was debrided. A similar decision-making process was applied to both isolated repairs and repairs in conjunction with ACL reconstruction.
We used the following scoring systems: (1) Knee injury and Osteoarthritis Outcome Score (KOOS) for symptoms and function in subjects;15 (2) Visual Analogue Pain Scale (VAS) from 0 to 10; (3) Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC);16 and (4) Single Assessment Numeric Evaluation (SANE).17,18 Recurrent tears revealed by new clinical signs or symptoms and requiring further imaging or return to theatre were recorded. Follow up was performed for a minimum of 6 months for all patients.
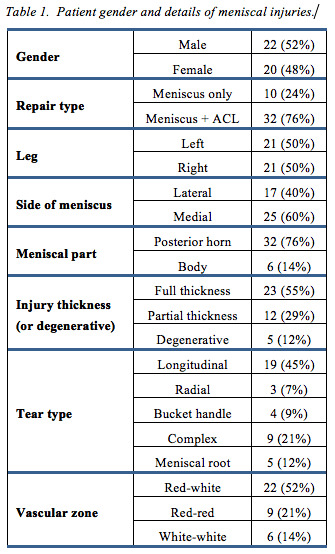
Details of the patients and injuries are shown in table 1.
Surgical technique An all-inside repair technique utilising the FAST FIX 360 ® device was used for each of the repairs. If the tear extended past the body of the meniscus into the anterior horn, inside-out and outside-in repair methods using the Meniscal Stitcher and Accupass Direct (Smith & Nephew, London, UK) were utilized in addition to improve access to the anterior meniscus and aid repair. We first identified the tear position and complexity in terms of the thickness of the meniscus involved and the type of tear as simple (single tear path) or complex (multiple tear trajectories). The decision to repair was based on surgical reparability rather than on predictions of vascularity or healing potential based on zone of injury. The tear was first reduced if required using a blunt probe and knee manipulation in the context of a displaced bucked handle tear. If visualization was impaired on the medial side, a fenestration was made in the deep fibres of the medial collateral ligament to provide safe access to the medial compartment. The tear was abraded with a meniscal rasp and arthroscopic shaver to facilitate a bleeding surface. For the all inside sutures, the instrument delivery needle was introduced through a split cannula. A vertical mattress configuration was used for all sutures. The needle first pierced the capsular side of the tear with anchor deployment, and the second pass pierced the meniscal side. Depending on tear configuration, a curved FAST-FIX 360 was utilized for a superior vertical mattress, and a reversed curved for an inferior. A probe hook was used to gradually reduce the repair followed by an arthroscopic knot pusher. The probe was then used to assess the stability of the sutureand a decision to proceed with further anchors was made. If the tear extended into the body or anterior horn of the meniscus, the Meniscal Stitcher kit with cannulae allowing introduction of loaded needles for Inside-Out orientation suture repair were used, or alternatively were passed Outside-In using the Accupass Direct Instrument. For repairs without ACL reconstruction, a microfracture of the intercondylar notch was performed to stimulate intra-articular bleeding and optimize the healing environment.
All patients were treated with a standardized rehabilitation protocol in a brace with full weight-bearing and unrestricted supine range of motion. Loaded range of motion was limited to 90° until 6 weeks, and deep squats were prevented until 3 months after surgery. Patients were followed up and evaluated using multiple scoring systems after 6 months.
Two patients required revision surgery for re-tears, one with an isolated medial bucket handle and the other with a combined ACL/Medial Bucket Handle repair. Both revision procedures revealed successful partial healing of the repaired menisci, with minor debridement of the non-healed component.
Data was analysed using SPSS for Windows software (International Business Machines,USA). P<0.05 was accepted as indicating statistical significance. The Levene statistic was used as a measure of heterogeneity of variance.
RESULTS
We identified 53 patients who underwent meniscal tear repair using an all-inside technique. Forty-two patients were analysed, having met the 6-month period of follow-up. Ten had isolated meniscal repair while 32 had concurrent ACL reconstruction. The age range was 13-65 years. cTwenty-two were male and 20 female, with equal involvement of left and right knees. Further details are shown in table 1. Three patients had meniscal root repairs and 5 had meniscocapular ramp lesion repairs (longitudinal tear of the peripheral capsular attachment of the posterior horn medial meniscus at the meniscocapsular junction. The number of anchors/sutures ranged from 1 to 9 per meniscus (mean 4.4). Of the 185 anchors utilised in the cohort, there was a total of only 4 failed FAST-FIX 360 anchor deployments in 3 patients and 1 failed Inside-Out Suture that necessitated intra-operative removal.
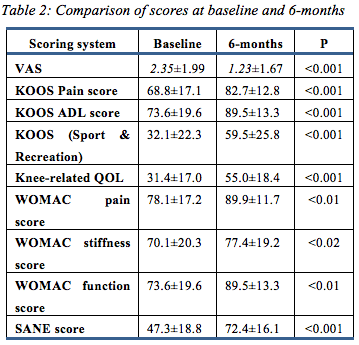
Pre-operative and 6-month VAS, KOOS, WOMAC, and SANE scores were assessed in all patients. All scoring systems recorded an improvement (table 2).
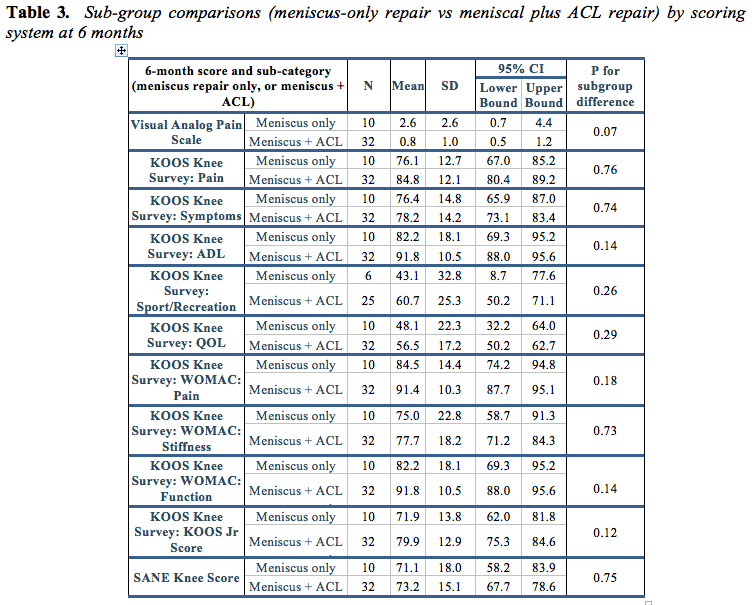
Comparisons between isolated meniscal repair and meniscal repair plus ACL reconstruction are shown in table 3. No significant difference was shown by any functional measure.
DISCUSSION
The most important finding of this study was the positive effect of meniscal repair seen across the cohort as measured by patient reported outcome and function. This was independent of concurrent ACL reconstruction, which has traditionally been considered to have an important role in optimizing the healing potential and success of meniscal repair. We recognize that a minimum of 6 months is a relatively short period of follow-up, but these findings are consistent with other studies that support ongoing longer-term benefit once a patient has successfully reached the 6 month mark. In a study of meniscal repairs using the FAST-FIX system, Pujol et al performed a 114-month average clinical and imaging assessment and reported objective International Knee Documentation Committee (IKDC) to be good in 92% of the cases.19 They concluded that an arthroscopic all-inside meniscal repair with hybrid devices will provide long-term protective effects, even if the initial healing is incomplete, due to the high strength of sutures.
Haas et al performed a prospective analysis using an all-inside FAST-FIX system. They evaluated 42 meniscal tears in 37 patients and 86% objective IKDC success rate. Both the subjective IKDC and the Lysholm scores improved statistically (IKDC average, 59 preoperative and 92 postoperative; Lysholm average, 69 preoperative and 94 postoperative). There were no postoperative extra-articular or intra-articular complications.12
Higher meniscal healing rates and improved outcomes in ACL-reconstructed knees may be due to increased blood flow in the joints from surgery, plus the more peripheral and vertical orientation of meniscal tears associated with ACL injuries.20 Furthermore, effective meniscal repair is an important part of ACL reconstruction, given that increased anterior laxity has been reported after posterior horn excision, the hypothesis being that the posterior horns are secondary stabilizers of anterior tibial translation.21,22 In contrast to this traditional belief, more recent literature shows similar success rates with isolated meniscal repairs compared to those with concomitant ACL reconstruction, as suggested by our data. In a 12-year analysis by Zimmerer et al, 73% of patients had successful surgery. Significantly better KOOS was found with isolated meniscus tears, but no differences in the failurerate comparing this group with those with simultaneous or delayed ACL-reconstruction.23 Another study by Bogunovic et al found no difference in the failure rate between isolated repairs (12%; 95% confidence interval [CI] -0.76% to 23.76%) and those performed with concurrent ACL reconstruction (18%; 95% CI: 7.5% to 29.1%). They also reported similar average time to failure between these two groups (48.1 months versus 46.6 months, p = 0.939).24 In a systemic review, Nepple et al reported that the failure rate was similar for both medial and the lateral meniscus as well as for patients with an intact and a reconstructed ACL. Their review demonstrated a very high rate of meniscal failure for a more than 5 year follow up period, for all techniques investigated.25 A recent study by Uzun et al reported outcome comparison for isolated meniscal versus concurrent ACL and meniscal repair. No superiority of concurrent meniscal and ACL repair over isolated meniscal repair was found.14 In our hands, the FAST-FIX system, though not subject to formal testing, proved reliable for all-inside meniscal repair.
Our study shows an improvement of KOOS scores comparable those shown in other studies.19,23 The importance of this study is the excellent short term outcomes after both isolated and combined meniscal repair. Aggressive meniscal repair guided by surgical reparability rather than a prediction of healing potential based on anatomical meniscal vascularity is therefore a valid part of operative decision making. Our study has confirmed that meniscal repair is likely to give excellent short-term results with or without ACL reconstruction, and isolated meniscal repair is a reliable and effective treatment option for patients with a reparable meniscus. We report a very low incidence of failed anchor deployment using the FAST-FIX 360 device and low rates of meniscal re-tear requiring re-operation. Excellent intra-operative tear visualization, meticulous surgical technique and utilization of appropriate tear specific repair methods are likely contributors to the successful outcomes seen in this study.
Subgroup cohort analysis was done to compare isolated meniscal repairs to those with associated ACL reconstruction. Due to heterogeneity of variance indicated by the Levene statistic, final subgroup analysis was done using independent t-test with unequal variation assumption and confirmed by Welch and Brown-Forsythe robust tests of equality of means. No significant difference was found between the meniscal repair groups with or without ACL reconstruction in any of the outcome scores at the 6-months evaluation period.
Our study is limited by the small group of evaluated patients and short term follow up. Longer follow up is required to confirm reliability and benefits of the procedure over time.
Corresponding author: Dr Navendu Goyal, Orthopaedic Research Foundation of Western Australia; c/o Fremantle Fiona Stanley Hospitals Group, Alma St, Fremantle, Western Australia, Australia. Navendu.Goyal@health.wa.gov.au
Disclosures: PD has received grants from Smith and Nephew Australia to travel and/or speak at surgical meetings unconnected with the study. Smith and Nephew Australia had no knowledge of the conduct of the study and did not participate in its planning or execution.
Funding: Not required
Provenance: Externally peer-reviewed









