Introduction
There has been a rapid global pandemic spread of SARS-CoV-2 virus (COVID-19). Viral particles which come into contact with mucous membranes lead to infection of respiratory tract epithelium and induce an inflammatory response that varies in degree but may be fatal.1 An important source of infectious particles is believed to be fomites that may be touched by potential patients or their doctors and transferred to mucous membranes by touch. Previous coronaviruses have been shown to be able to live on surfaces for 48-72 hours.1-3
Good hand hygiene is important for infection control in healthcare environments, and abstaining from face touching has been highlighted by public health authorities as an important measure to reduce transmission of COVID-19. Self-inoculation occurs when contaminated hands or objects touch facial membranes.1
Most people are unaware of how often face touching occurs.4 A study of UNSW medical students reported an average of 23 face touches per hour4,5 and a study of health care practitioners showed no difference in face touching between those health staff who reported actively practicing behaviours to minimise the chance of URTI and those who did not (19 versus 20 touches over 2 hours of observation).6
Risk factors for self-inoculation are the rate of face touches, rate of contact with environmental surfaces, how contaminated these surfaces are, and the pathogen virility.7 Current literature is not clear on the reduction in face-touching behaviour required to reduce the risk of self-inoculation with coronavirus. The aim of this audit was to observe the rate of face touching in ICU medical teams during their morning ward rounds and to determine if an education intervention reduced this rate on re-audit.
Methods
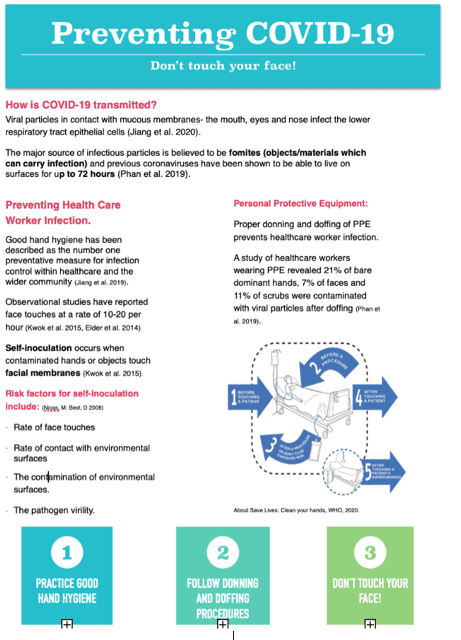
A literature review was conducted on Google Scholar and Pubmed using the keywords face-touching behaviour, COVID-19, intensive care and hand hygiene. An educational handout (Figure 1) was produced and distributed to members of the ICU clinical teams (n = 6). The teams read the handout and questions were answered. Subsequently, the teams were observed without notice for face touching behaviour at non-isolation beds for one hour and the number of touches amongst medical staff present, observed simultaneously, were recorded. A touch was classified as contact between the palmar surface of the hand to the face categorised into eyes, lips, nose or non-mucosal surfaces. Touching of spectacles was regarded as non-mucosal. The teams were approached and advised of the audit. The same team was then re-audited for 1 hour the following day.
The ICU teams were rostered to the ICU ward for the week. This enabled study of the same participants on both study days. A participant was included in the study if present for 40 minutes or more of the observation period on both days. Facial masks and whole body personal protective equipment (PPE) had not been mandated during the study period and were not used outside isolation rooms. At the time of the audit, gloves were not mandatory in the general ICU ward and were not worn by any of the staff studied at non-isolation beds.
Data was collated on Microsoft Excel and analysed using STATA V16.1. Wilcoxon-signed rank test was used to evaluate pre- and post-intervention face touching and the Mann-Whitney test evaluated the differences in face touching after education by gender and spectacle wearing.
Ethical approval was not required for this audit, as determined by the Northern Sydney Local Health District Human Research Ethics Committee, in line with the National Statement on Ethical Conduct in Human Research.8 The audit was conducted from April to May, 2020.
Results
Twenty-two intensive care doctors from six intensive care teams were observed over five weeks. Eighteen (8 female, 10 male) satisfied the inclusion criteria. Six doctors wore spectacles. Nine were observed in the COVID ward and the same number in the general ICU ward.
There was a significant reduction in the number of observed face touches from a mean of 12 per person before to 4.5 per person (range of paired differences, 5−17; p = 0.009) after the intervention.
Females tended to reduce face touching behaviour more than males (Mean reduction 10.4 compared to 4.75, respectively), but the difference by gender was not statistically significant (p = 0.23). There was no significant difference between individuals wearing spectacles (p = 0.35) or individuals working in COVID versus non-COVID wards (p = 0.27).
Discussion
The COVID-19 pandemic has had a major impact on healthcare worker perception of self-risk and their capacity to deliver optimal care to their patients. This has led to increased efforts in favour of standard hygiene practices such as PPE use. The medical teams reported a high awareness of face touching and its significance, and most participants changed their practice during the audit. We demonstrated a significant reduction in face touching behaviour 24-hours after distribution of the information pack. The reduction was not statistically gender-related but this may be a consequence of the numbers studied, and was the same in doctors who wore or did not wear spectacles. It is reasonable to regard the observed reduction in face touching as potentially clinically significant with regard to COVID-19 infectivity.
The change occurred rapidly but its duration was not studied. For a behaviour that is learned through life, long lasting change is likely to require re-education, and re-auditing the study individuals would provide further information on this point.
This study has several important limitations. The sample size was small and the ‘before and after’ design lacks a positive control. Bias on re-auditing was possible, as staff were potentially aware of the second period of observation, introducing the possibility of a “Hawthorne effect” on the results. Staff participants could not always be observed for the full hour as ward rounds are dynamic, and continuous observation was not possible if staff moved to staff different ward areas or while examining patients with curtains drawn. Thus some face touching behaviour may have been missed. Lastly, the study was time-limited and the long-term behavioural effect if any is speculative.
Increased use of PPE in response to COVID-19 within the healthcare environment since this audit was undertaken may have reduced the risk of self-inoculation associated with face touching behaviours.
Conclusion
Face-touching behaviour of intensive care doctors was significantly altered and the number of face touches fell after an educational intervention during morning ward rounds in the ICU. Which component of the exercise (staff knowledge of the intervention, the distributed educational material or the audit itself] is uncertain, but the audit process was a useful tool for direct feedback to teams on their performance. Staff members were receptive to advice, agreed with the need to modify their behaviours, and did change face touching practices in the short term.
We acknowledge that the study has important limitations as outlined above and that further studies are required to confirm the positive findings and define the duration of the effect.
Provenance: Externally reviewed
Ethical Approval: Not required (see text)
Declarations: None
Corresponding Author: Dr Kirsten Rowcliff, Royal North Shore Hospital, St Leonards, NSW, Australia. Email: Kirsten.rowcliff@health.nsw.gov.au









