Introduction
Virtual fracture clinics (VFC) are established in the United Kingdom as a cost-effective conservative management pathway for patients with uncomplicated fractures.1,2 In a VFC, such patients are streamed to clinics staffed with advanced scope physiotherapists (ASP) and experienced nurses working in collaboration with orthopaedic surgeons. Many injuries that can be managed in boots, splints and slings are streamed to discharge with information or telephone follow up clinic.3 The primary rationale of establishing a VFC is to free up surgeons to review patients with more complex injuries who may require surgery.4 Secondary benefits to patients and the orthopaedic service include reducing the time to specialist review, reducing the number of plain radiographs, convenience and satisfaction for the patients and reduced cost of fracture management.3
The efficacy of a VFC has been well demonstrated in adult populations5 and there is emerging evidence for including paediatric injuries.6 A UK audit of paediatric fracture referrals to specialist outpatients found that a third of patients had no fracture on x-ray and 20% of the referrals were for uncomplicated ankle and finger fractures requiring minimal intervention.7 The challenge with a paediatric population is to identify patients who need further urgent review and investigation, even if the initial radiograph shows no fracture.8
The driving forces to establish virtual fracture clinics in the UK were reduced treatment costs, streamlined patient services and reduced outpatient clinic overbooking.9 The Australian and UK health care systems share many characteristics, as universal free hospital care underpins both hospital systems. We also face high costs of care, and problems of ongoing patient rehabilitation and a progressive increase in patient numbers. Internal audit of 5th metatarsal, radial head and clavicle fractures and comparison with published data on the VFC management of these injuries4,5,9 suggested a potential opportunity for a VFC. Health economic analyses of physiotherapist-led orthopaedic triage services in sub-acute and chronic patient populations also support potential VFC cost-effectiveness with an acute patient cohort,10,11 especially if the innovation is associated with other changes, such as patient-focused bookings,12 where patients determine their need for an appointment.
To create a VFC within the orthopaedic service in our hospital required significant changes in clinical practice. We had to address issues of clinical governance, staff training and support of physiotherapists in a new advanced scope role, changes to well-established administrative processes and creation of new communication channels with patients. In doing so we wished to maintain the current high standard of outpatient clinic level of care, and we were aware that our patients may require explanation over what is meant by a “virtual model of care.” We drew heavily on the established NHS VFC models of care, but it was not our intention to copy. Rather we felt it likely that our VFC would develop its own character as a result of detailed differences in the two jurisdictions.
The existing literature describing VFCs reflects the operational requirements and patient demographics of current mature UK services. We explore here the patient demographics and operational challenges of our new VFC service at Fiona Stanley Hospital.
Methods
In May 2020, we established a VFC orthopaedic service at Fiona Stanley Hospital (FSH), following the model from Brighton and Sussex NHS Trust. FSH is a tertiary teaching hospital with 780 beds located in the southern suburbs of Perth, Western Australia. This is a descriptive analysis of data collected from the first 8 weeks of VFC operation (18 May 2020 to 13 June 2020).
Clinical governance in the VFC is managed by registrars on the orthopaedic surgery training program designed and regulated by the Australian Orthopaedic Association. The registrars are direct clinical supervisors of the ASPs working in the VFC. In the initial piloting phase the ASPs were required to discuss all decisions required within patient management plans, radiology interpretation and change of clinical management with the registrars. All ASPs had considerable experience in managing fractures (as primary practitioners in the emergency department), but had limited experience in orthopaedic outpatient settings. They managed patients selected for the VFC independently unless the patients deviated from their expected recovery trajectory.
Triaging patients to the VFC
Referral triage was conducted by the ASPs. They screened the list of patients referred to the Orthopaedic service each weekday morning and presented VFC-suitable patients to the registrars who made the final streaming decision. A management plan was agreed at the time of triage. The daily referral streaming decisions were recorded as this will be used to determine the scope of the VFC as it transitions out of the pilot phase. The current effective scope of the VFC is based on the ASP and registrars’ collaborative clinical decision-making.
Inclusion criteria
Patients of all ages referred from all referral sources (e.g. General practitioner, Emergency Department, H.M. prisons); Acute traumatic injury; Injuries with good prognosis on uncomplicated conservative management (e.g. fractures of clavicle or 5th metatarsal; buckle fractures; undisplaced radial head fracture); Referrals not normally managed by a tertiary orthopaedic service and suitable for physiotherapy (e.g. ankle sprains).
Exclusion criteria
Requirement for surgery; Absence of suitable English language skills; Requirement for further physical examination to establish diagnosis; High-risk injury types (e.g. paediatric elbow injuries, carpal injuries, tarsal injuries)
Patient contact and bookings
All VFC patients had appointments with the ASPs either by telephone, video call or face to face, depending on clinical need as determined by the management plan agreed with the overseeing registrar. When contacting patients, the ASPs identified themselves as physiotherapists, explained the role of the VFC, identified patient concerns and expectations and conducted whatever physical examination was possible under the circumstances, guiding the patient where necessary. Patients were provided with an information sheet about their injury, including relevant exercises, treatment and likely prognosis over a 12-week recovery timeline. Many patients had a single telephone appointment, however follow up for each patient was agreed between the patient and the ASP depending on the identified needs of the patient.
All patients were provided an e-mail address and a direct phone number to the VFC to provide additional service or support. We positioned the VFC as a partner in helping patients to manage their injury and welcomed repeat contact. We assigned to patients the privilege of determining the support they needed and when it was required,12 rather than automatically booking multiple appointments. The clinic business rules allowed clerical staff to book VFC patients for review on request by phone or email and a separate email address was provided. This process gave additional support to patients.3
Retrospective audit
We audited retrospectively the clinical data collected routinely during the first 8 weeks of the VFC. All patients were registered on a REDCap database (Vanderbilt University) that included patient and clinical progress information with underlying treatment decisions. The database also captured information on referrals that were not deemed suitable for VFC management to help explore the boundaries of scope for this clinic.
This audit also included the number and type of clinical encounters in the VFC (drawn from the FSH patient management system (WEBPas)) and the rate of clinical imaging from the radiology system (PACS). We performed a descriptive analysis of the data.
This data collection process is part of our hospital registered Quality Improvement process (Reference GEKO 35578).
Results
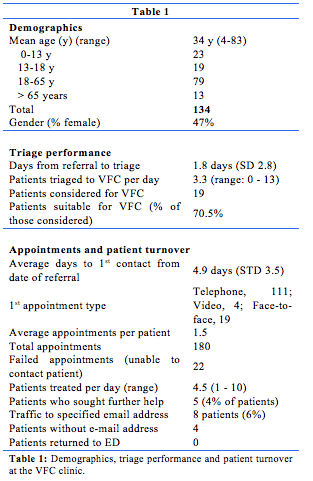
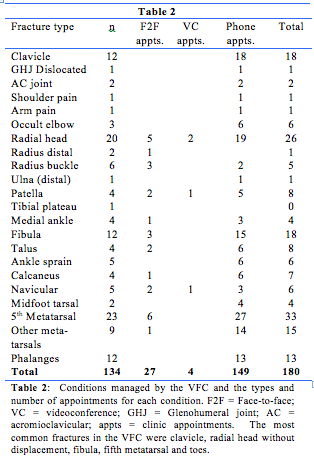
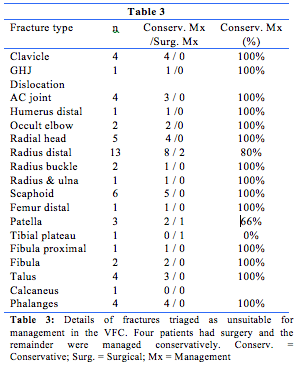
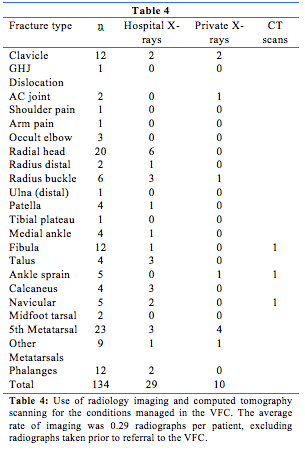
Clinic workload, performance and achievements are shown in tables 1 to 4.
Discussion
Launching a VFC within an established orthopaedic outpatient service has been a challenging process. We believed it essential for success that a mature and established ASP workforce was available to provide staff in the VFC. This experienced workforce comprised primary contact clinicians used to making patient treatment decisions and working independently in a medical substitution role. To establish this workforce in Orthopaedic outpatients we secured pilot project funding from the South Metropolitan Health Service through their innovation program. With the funding we were able to establish a 0800−1230 weekday outpatient presence.
In establishing the clinic, we had to extensively brief the outpatient clerking team, outpatient nursing team, hospital call centre and emergency department on the VFC. We had to establish new administrative processes and find a workspace in a very busy outpatient clinic. We set up a RedCAP database that acted as a data collection tool, but also as a communication tool between the 3 ASP working in the VFC. We found that the electronic medical record was not suitable for recording decisions on patient management made with the registrars. We had a number of early technical issues with video calling and quickly discovered that patients are more likely to answer a phone call if they can see the caller’s number (most hospital numbers are hidden). We changed our main call number to display to patient telephones as a result. The dedicated VFC phone number was set to default to the main hospital outpatient call centre outside VFC clinic hours.
The establishment of this VFC was strongly influenced by the model used in NHS trusts in United Kingdom. Our age range of 4-83 seems in keeping with the scope of some virtually managed injuries,4,13 but different to the overall scope of the Edinburgh Trauma Triage Clinic which sees patients 12 years and older.5 Our experience is that paediatric fractures require careful consideration, though some are clearly suitable for VFC review (e.g. clavicle,6,14 metatarsal,6 lateral malleolus6 and torus fractures of the distal radius15). However, others such as some elbow fractures6,8 may not be as clear cut.
The average time to triage from receipt of a referral was 1.8 days. Referrals were triaged at the beginning of every clinic day, and the longest delays typically relating to weekend referrals triaged on a Monday. We averaged 3.3 patients triaged to the VFC each day, with no suitable patients on some days and up to 13 on others. Typically, Mondays had the most referrals from the Emergency Department and a higher ratio of suitable patients. A recently established Australian Tertiary Hospital VFC with consultant led triage reported a 33.5% rate of triage to the VFC from ED.16 Triage rates of 35% have been reported in Ireland.17 We have not been able to measure our triage rate as the VFC was not set up as a separate clinic on hospital patient management systems, but estimate that 0-25% of all Orthopaedic service referrals were triaged to the VFC each day.
The average waiting time to a first appointment from the date of referral was 4.9 days. The wait is often dictated by the treatment plan, as some patients may be contacted on the day of triage while others require time for the injury to settle allow re-examination. Having an early first appointment can reduce patient anxiety18 but clinical and radiological requirements may require some delay. Our average time to first appointment falls outside 72 hours which is a benchmark in the United Kingdom.18
Eighty-three percent of VFC patient initial appointments were by telephone. Four patients (3%) had a video call as the initial appointment. Using video technology is an effective way of examining patients clinically, and our limited use reflects technical challenges we faced in adopting this technology. Fourteen percent of patients had the initial appointment face to face. This is in keeping with reports from other VFCs where the need for face to face appointments were dictated by the use of plaster in ED,6,15 patients needing a brace6 or the injury type (e.g. hand and wrist injuries3,20). Establishing well-defined injury management protocols should improve our future efficiency.9,15
Patient contact at the appointment time was unsuccessful on 22 occasions. Many patients did not expect a telephone contact or had incorrect contact details on the hospital record. This is higher than at a comparable Australian service which reported a 6%16 unable to contact rate. Including these unable to contact events, we conducted 202 appointments and averaged 1.5 appointments per patient. Most patients required only a single contact from which they were discharged with self-management advice. Review of appointment numbers shows a difference between the Australian style of VFC and the UK model. For example, average appointment numbers per patient with a 5th metatarsal fracture were 1.22 in our service, 1.06 in another Australian VFC16 and 0.17 in a UK VFC (5th metatarsal).9 Every patient in our VFC has one formal contact, where in the UK there is a high rate of direct discharge of referrals, with information posted to the patient.20
Triage in our clinic is a shared process between the ASP and surgical registrars. One hundred and ninety patients were referred, and 134 (70%) were triaged to the VFC. Our casemix (Table 2) reflects that reported by mature VFC services. We are strongly aligned in our inclusion of clavicle,3,6,14,17,21 radial head,3,5,18,20,21 distal fibula,6,13 metatarsal,3,5,9,17,21 toe, distal radius torus fractures6,15,17,21 and injuries without radiological evidence of injury.6,21
While most VFC models are consultant-led, in our model the triage decision-making is by surgical registrars on the orthopaedic training program. We have reviewed our cases for evidence of adverse events and found no return to the emergency department, no re-referrals from primary care and no additional patient contact with the hospital (including complaints) outside the established VFC pathways. No VFC patients returned to the emergency department, which compares well with a published rate of 1.9% re-attendance in a VFC established in Glasgow, Scotland.22 Thus we believe that our model is safe despite the delegation of decision-making to trainees.
Amongst 56 cases deemed unsuitable for VFC management we identified 4 patients who progressed to surgical intervention (Table 3). The remaining patients continued with conservative management, suggesting that some may have been suitable for the VFC pathway. Our patients are accustomed to attending a face-to-face appointment with an orthopaedic surgeon, and triage may have been affected by this custom. This is especially true with paediatric patients. The area with the largest scope to increase VFC patient numbers is hand and wrist injuries,19 particularly fifth metacarpal fractures.5,23 Other possible injuries are tendinous injuries including mallet fingers and Achilles tendon rupture.24
Table 4 shows the rate of imaging for patients of the VFC. The overall rate of 0.29 new radiographs per patient is reflective of a small number of injuries needing radiographs to demonstrate stability or to review healing. One unsolved challenge, particularly as our pilot coincided with COVID community movement restrictions, is providing patients managed by telephone consult with follow-up imaging without footfall in the hospital.
This study has several limitations. The recovery period for patients with fractures extends beyond the period of study out to 3-6 months and we do not have longitudinal data on patient outcomes at these time points. In a VFC treatment pathway routine collection of functional outcome data will be important as an auditing tool, to establish efficacy and cost-effectiveness. Economic benefit needs to be established for this pilot project to progress to permanent establishment. We write from a health service perspective, but given the importance of patients as partners in their own care, future research should include patient perspectives on the model of care. Providing information on injury self-management is also vital to this virtual process and further research is needed on how best to present this for patients with variable literacy.
This review has highlighted several areas for potential improvement. We anticipate increased efficiency as the administrative and clinical staff become accustomed to the new treatment pathway. The ASP new to this clinical environment will also become more efficient with further training and exposure. Our biggest gains are likely to come from developing algorithms for the treatment of common fractures with good prognosis, under conservative care.25 We also hope the collection of detailed patient demographic data for the VFC will identify key metrics for other services considering establishing similar services.
Provenance: Externally reviewed
Ethics approval: Not required
Declarations: None
Acknowledgements: We are indebted to Dr Kit Brogan, Brighton and Sussex NHS Trust, Dr Clarice Tang, Dr Andrew Mattin, Dr Hannah Seymour, Paul Forden and the innovation team at the Southern Metropolitan Health Service.
Corresponding Author: Dr Piers Truter, Orthopaedic Service, Fiona Stanley Hospital, Murdoch, WA 6150, Australia. Email: Piers.truter@health.wa.gov.au
