Introduction
Risk stratification of patients undergoing non-cardiac surgery is vital to minimize peri-operative adverse cardiac and cardiovascular outcomes.1 Integrated multimodal evaluation, including functional assessment, cardiovascular risk calculation and surgical stress categorization, appears to be a better predictor of adverse cardiac outcomes than single mode review.2 Surgery causes myocardial stress and increases cardiovascular risk and mortality.3 However, myocardial stress and damage during peri-operative period may be asymptomatic due to several other factors such as the use of opiate and other analgesics.4 Therefore, biomarkers appear to be better predictors of myocardial damage across all types of surgical procedures, as described in the 4th universal definition of myocardial infarction (2018).5 Amongst those predictors, troponin and brain natriuretic peptide (BNP) are the main biomarkers investigated to date.6 Troponin measured after non-cardiac surgery is better in detecting myocardial infarction than in prediction obtained pre-operatively.7
Preoperative BNP has also been studied as a predictor of adverse cardiac outcomes and mortality after major surgical procedures.8 BNP and its inactive form, N-terminal prohormone BNP (NT-proBNP) are released from cardiac myocytes in response to myocardial stress.9 Serum concentrations of BNP/NT-proBNP can be measured in peripheral blood. Several meta-analyses and systematic reviews have demonstrated that BNP/NT-proBNP levels predict adverse cardiac outcomes including non-fatal myocardial infarction, cardiac death after non-cardiac surgery, and non-fatal myocardial infarction at 30 days after surgery.10-15 I review here the role of elevated BNP in perioperative risk stratification for non-cardiac procedures. Priority was given to prospective studies that investigated BNP/NT-proBNP prior to non-cardiac surgery and its prognostication ability for adverse outcomes.
Pathophysiology of BNP release
BNP is a small protein molecule belonging to a group of hormones called ‘natriuretic peptides’. Other members of the group are atrial natriuretic peptides (ANP), C-type natriuretic peptide (CNP), and Dendroaspis natriuretic peptide (DNP).16 In fact, DNP can be detected in human plasma and atrial myocardium in heart failure, but its role has not been fully elucidated.17 Dilatation and stretching of ventricles from various physiological and pathophysiological states cause release of BNP to blood stream. Some of the causal factors for ventricular dilatation are volume overload, sympathetic stimulation and inflammatory response in the peri-operative period.18 The inactive prohormone of BNP (N-terminal pro-hormone BNP or NT-proBNP) can also be detected in blood and gives rise to BNP by cleavage of the 76-amino acid N-terminal peptide. The physiological ANP and BNP effects involve reduction of renal salt and water reabsorption, leading to polyuria, natriuresis, and decreased circulatory blood volume.9 Raised plasma BNP/NT-proBNP is evident predominantly in heart failure and other situations of ventricular dilatation and intraventricular pressure (Fig. 1). Patient age, body mass and renal function also contribute to increased BNP/NT-proBNP.6
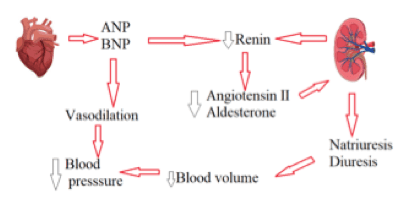
Pre-operative hypotension is associated with increased post-operative mortality.19 During surgery, various mechanisms could increase BNP levels and be responsible for hypotension. However the evidence for BNP-driven hypotension as a cause of adverse outcomes is difficult to prove as other mechanisms for peri-operative hypotension such as blood loss and anaesthetic drugs are often present.
Current evidence on BNP as a predictor of surgical risk
I searched the literature search for original studies published on BNP or NT-proBNP in peri-operative cardiovascular risk stratification. Reviews were not included. Several large-scale prospective studies were identified.
A prospective study of pre-operative BNP (>189 pg/ml) levels evaluated adverse cardiovascular events in 1590 patients undergoing non cardiac surgery. There were 21 cardiac deaths, 20 cases of nonfatal myocardial infarction, and 41 cases of acute pulmonary oedema, with total event rate of 6%.20 Another smaller study assessed 41 high risk patients with moderate to severe pre-operative cardiac failure (ejection fraction <40%) or severe aortic stenosis undergoing vascular surgery. Mean BNP of 1366± 1420 pg/mlwas noted in patients with adverse cardiac events compared to 167 ± 194 pg/ml in patients without adverse events.21 Similar findings were observed in 279 elderly patientsundergoing non-cardiac surgery.22 NT-proBNP levels >201 pg/ml was independently associated with high incidence of peri-operative complications. The sensitivity and specificity were 80% and 81% respectively. NT-proBNP levels were also associated with cardiovascular risk.22
A study of 2519 patients over 59 years of age undergoing emergency non-cardiac surgery assessed risk of adverse outcomes using pre-operative BNP and troponin (cT). The major adverse cardiac event rate of 10% was independently associated with preoperative BNP and cT (P <0.001).23 There was a close relationship with pre-operative BNP levels and cardiovascular events post-operatively even in low-risk patients.24
Though almost all studies have demonstrated a statistically significant association between BNP/NT-proBNP and major adverse cardiac events after non-cardiac surgery, the challenge is to identify a threshold concentration above which a patient is at unacceptable high risk of cardiac complications. However any threshold value is likely to have poor sensitivity and specificity. In the above studies, patients with BNP as low as 36 pg/ml had adverse cardiac outcomes.25 A wide variation in BNP units of measurement and cut off values existed in these studies. Heterogeneity of available BNP assays, half-life differences between BNP versus NT-proBNP and variability of study cohorts by surgical and cardiovascular risk could have contributed to this variability.26 In addition, physiological biomarkers may vary in their response to the pathophysiology arising during surgery, and this may affect their use as predictors of risk.
Current recommendations on BNP in perioperative care
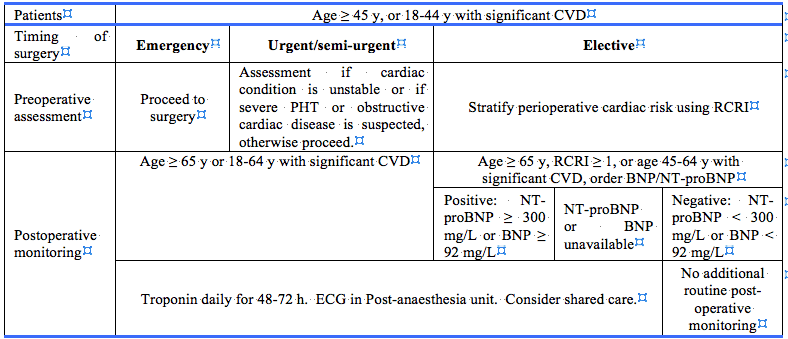
Major guidelines currently provide limited recommendations for the usage of BNP in peri-operative setting (Table 1). The American College of Cardiology and American Heart Association do not currently mention use of peri-operative BNP for risk assessment. This is due to factors such as variable timeframes of BNP used in studies, limited randomized data and lack of guidelines for treatment when biomarker concentrations are abnormal.27 However, the Canadian Cardiovascular Society (CCS) guidelines recommend BNP or NT-proBNP in high-risk patients undertaking elective surgery, defined as patients aged 65 years or older or patients aged 45 to 64 with cardiovascular risk factors.28 Cardiovascular risk was calculated based on the vascular history or a point in the Revised Cardiac Risk Index (RCRI). This was further described according to the timing of surgery in the CCS guidelines (Table 2).
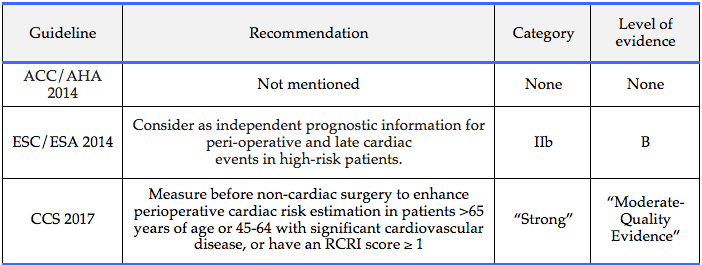
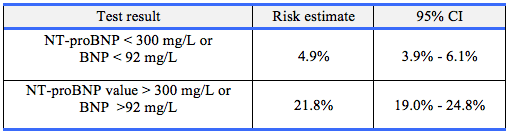
Furthermore, the CCS provided risk estimation of death or myocardial infarction within 30 days after non-cardiac surgery based on pre-operative BNP and NT-proBNP levels (Table 3). The European Society of Cardiology and the European Society of Anaesthesiology (ESC/ESA) guidelines mention pre-operative BNP/NT-proBNP merely as an added prognostic factor for predicting adverse cardiac events.27 Application of BNP/NT-proBNP as an independent predictor for peri-operative and late cardiac events, was able to provide only class IIb level of evidence. Routine use of biomarkers is not recommended in ESC/ESA guidelines.29
No studies that considered or demonstrated the cost-effectiveness of BNP/NT-proBNP in perioperative risk stratification and prognostication were identified in the search. Widespread pre-operative measurement of BNP/NT-proBNP on empirical grounds would be costly and unlikely to be cost-effective. This contrasts with the situation in heart failure, where routine BNP monitoring compared to a symptom-based approach is cost effective.30
Conclusion
Almost all available randomized studies have demonstrated a positive relationship between pre-operative BNP/NT-proBNP levels and adverse post-operative cardiac outcomes. Therefore BNP/NT-proBNP are useful biomarkers for predicting adverse outcomes after a surgical procedure. However it is difficult to find a precise level of BNP which predicts the adverse event risk with acceptable precision. As a result, the use of BNP in perioperative risk assessment remains uncertain. Major international guidelines disagree. Current recommendations and major guidelines are based on limited available evidence, and further large-scale randomized studies are required to achieve a standard guideline.
Ethics approval: Not required
Conflicts of interest: None
Funding: Not required.
Provenance: Externally reviewed
Author’s address: Dr MT Iddagoda, Department of Geriatric Medicine, Royal Perth Hospital, PO Box X2213, Perth, Western Australia 6847, Australia.









