INTRODUCTION
When admitted to a hospital due to an acute illness, elderly patients who are at greater risk of multimorbidity may loose essential skills to undertake the activities of daily living (ADL) and therefore their independence,1,2 not only due to the acute illness that led to the admission but also due to the lack of individual therapeutic management.3 Covinsky et al demonstrated that up to 50% of patients older than 85, had a lower function in the ADL after hospital admission than before the acute illness.1 In consequence these patients potentially cannot return to their home, and are likely to be institutionalized.
Hospital care settings should be aware of the risk of additional loss of independence that patients may endure during their hospital stay.3 Special geriatric knowledge and a multidisciplinary team approach to maintain the functional status of the patients during their hospital stay are some of the factors that might prevent irreversible decline of function in the ADL. These patients often need rehabilitation after an acute illness, injury or surgery to regain their functional autonomy.
The study had two aims:
1. To identify if other patient characteristics such as being married (as proxy for living with someone), gender and age, influence the prediction for the discharge location by the Functional Independence Measure (FIM) score.
2. To validate the clinical observation that some specific FIM items seems particularly important in predicting discharge to home.
METHODS
Our rehabilitation facility is part of the public hospital (HFR) in the canton of Fribourg (population 318,000) Switzerland. All patients admitted to the facility from August 2005 to December 2012 for 7 or more days and discharged to home or an aged-care facility were included. Exclusion criteria were death during admission, discharge to any acute hospital (somatic, psychiatric, and geriatric) or other rehabilitation facility and unknown discharge location.
Demographic data was retrieved from the hospital administrative database (OPALE). Age, gender, marital status, length of stay, discharge location, FIM scores on admission and discharge were collected. Incomplete data sets were excluded from the statistical analysis. The study data was anonymized by the principal investigator before being sent for statistical analysis.
All patients received a multidimensional assessment on the basis of the bio-psycho-social model. Medical conditions and medications were reviewed and all received physio- and occupational therapy adjusted to individual functional and cognitive disabilities and personal goals. Depending on need patients also received speech therapy, nutritional counseling and neuropsychological evaluation. Our social services help with the discharge planning and organize any additional assistive equipment needed.
A first FIM evaluation was undertaken within 72 hours of admission. Treatment goals are defined discharge planning is started with patient involvement. The FIM® instrument consists of 18 items; 13 for motor and 5 for cognitive function. The scores range from 1 (total dependence) to 7 (complete independency) per item, thus the score ranges from 18 to 126 points. A minimum of functional autonomy is required for a patient to be able to return to his home. A patient living alone, requires higher motor and cognitive skills than a person living with a spouse or other carer.
In order to enable the patient to participate and undertake activities of his/her choice, specific goals to achieve during rehabilitation were established. For a person not living alone, a score for the above activities of above 3 (needing some physical support) can be sufficient for home discharge. Significantly lower scores in the cognitive functions can be tolerated as well, as a caregiver is present. That person can also assist with other activities of daily living, which are therefore not vital.
The achievement of these goals and measurement of functional status were assessed weekly and discussed during an interdisciplinary meeting and adjusted as required. Furthermore at least one meeting with the family and other persons involved in the care of the patient after rehabilitation was organized to discuss discharge dispositions. When necessary, the occupational therapists undertake a home evaluation to assess the need for adjustments to be made in the home environment, for higher safety.
The FIM score was re-evaluated 72h before discharge and all essential external help was organized. Social workers assisted the patient and his family with administrative work required for discharge, such as registration for admission to nursing home.
Approval from the Swiss ethical committee in Lausanne was granted on the 13th October 2014.
Statistics
Statistical analyses were performed using SPSS V20 (IBM) was used. Logistic regression was used to assess the influence of each FIM sub-score as well as age, sex and marital status on the probability of being discharged home or to an institution. Each of the FIM scores was expressed as standard deviation (SD) units in order to allow comparison of odds ratios between different parameters. Age was expressed in decades. Both univariate and multivariate analyses were conducted. Univariate analyses contained only a specified variable, while multivariate analyses included all variables including interest, age, sex and marital status. The interaction between marital status and other variables was also tested as this was hypothesized to be a moderating factor. The reported odds ratios for all FIM scores are for a one SD change in the FIM score.
RESULTS
A total of 2585 patients were admitted to the rehabilitation facility during the study. After application of exclusion criteria, 2218 were enrolled into the study. Complete information was available for 1727 patients. Of these, 1386 (80.3%) returned home and 341 (19.7%) were discharged to a nursing home or similar institution. The final study sample comprised 1118 women (64.8%) and 608 men (35.2%). The mean age of patients discharged home was 77.8± 9.9 (SD) and 83.4± 7.86 years for those discharged to an institution.
Patients admitted to our rehabilitation facility have a variety of indications and their mean age ranges from 67-90 (mean age of 79) with slightly more women than men (approx. 63% vs. 47%). More than 80% of the study population was discharged home after an average length of stay (LOS) in rehabilitation of 22 days (interquartile range = 14 – 27 days). Patients discharged home were younger (77.7 vs 83.3), mostly female (63%) and living alone. Table 1 shows the demographic data, baseline and discharge characteristics. The unadjusted OR and p values showed a significant influence for gender.
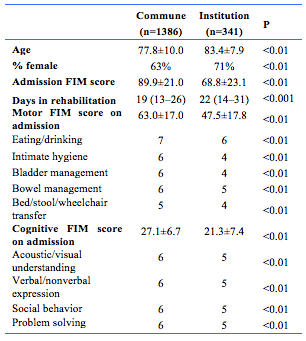
Those discharged to nursing homes vs home tended to stay 3 days longer in rehabilitation (25 vs 22 days) and had lower FIM scores at both admission and discharge. They also had a smaller increase in total and motor FIM scores during their stay, but the change in cognitive scores or its sub-scores was not significantly different (table 2).
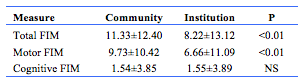
Table 3 shows the results from the univariate (age, marital status, gender, FIM Scores) and multivariate (FIM sub-scores) analyses of risk factors measured at admission. Older age reduced the odds of being discharged home. The data confirmed that autonomy in eating/drinking, intimate hygiene and being able to transfer independently are significant motor skills for discharge home. Analyses adjusted for age, gender and marital status showed congruent patterns to the unadjusted analyses, although the beneficial effect of female gender on discharge home was no longer significant.
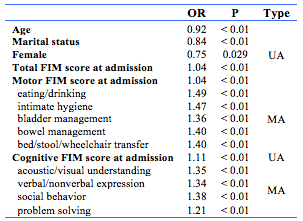
The discriminative ability of the change in FIM scores was low compared to absolute admission or discharge values. Acoustic/visual understanding and social behavior, closely followed by expression (verbal/nonverbal) were most significant cognitive function sub-scores for discharge home.
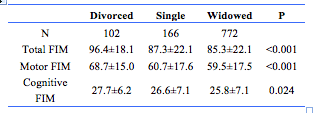
FIM scores at admission were higher (p=0.039) for patients living alone (n=1040; 86.7±21.9) versus currently married patients (n=686; 84.4±24.5). Table 4 shows for patients living alone that divorced patients exhibited significantly higher total FIM scores and greater functionality than either singles or widowed patients.
DISCUSSION
C V Granger and his co-workers, in a joint task force appointed by the American Academy of Physical Medicine and Rehabilitation and the American Congress of Rehabilitation Medicine, created a uniform data set for measuring disability and rehabilitations outcomes in 1983. As a result the Uniform Data System for Medical Rehabilitation (UDSMR) was created. The UB (University at Buffalo South) received a three-year grant in 1984 from the National Institute for Disability and Rehabilitation Research to develop such a standard.
The UDSMR, the FIM instrument and UDSMR data-management service are the result.4Fifteen years after Faculty members in the UB Department of Rehabilitation Medicine created the FIM instrument, they were involved with the federal Health Care Financing Administration (HCFA) in developing an instrument to be used by rehabilitation hospitals and other rehabilitation units as the basis for Medicare prospective payment in 1998.
The FIM score has since become the most frequently used assessment tool in the USA5 and has become a means of estimating payment to inpatient rehabilitation facilities by insurance companies. Several studies have demonstrated a relation between FIM discharge scores and discharge location.5-7 Most are based on a specific sub-population of patients – for example, those with stroke5,6 or hip fractures.8 This study was in an unselected sample of elderly patients in the rehabilitation facility and thus may have wider application.
Reistetter et al found a cut-off value for total FIM score of 78, above which a patient could return home,6 whereas the review by Bottemiller et al cited several articles suggesting that FIM score on discharge >80 gave a 90% chance of returning home, compared to scores < 40 where the corresponding chance was only 30%. It remained unclear what happens to those with an intermediate score.
Most studies have been conducted on selected patient populations8-13 Seematter et al examined a more heterogeneous patient sample, but employed the Barthel Index.14 Other studies have included heterogeneous patient populations15-17 but to our knowledge this is the first study in an unselected patient population to evaluate the utility of the FIM Instrument in the discharge planning of a broad selection of patients.
Several studies13,15-17 aimed to identify predictors for the discharge location. Although most found that motor13,16,17 and cognitive13,17 skills were important predictors, Astell et al found that independence for ADL was the key predictor.15 This is consistent with our findings for the specific FIM motor subscore, similarly established by Jackson et al who identified 3 physical performance items (grooming, toileting and chair transfers) as well as 4 cognitive performance items (comprehension, expression, problem solving and memory) as predictors.17 Shashi et al were also able to identify predictors similar to ours: age, gender, cognitive and motor skills,13 but others found age to be a weak predictor.15,17
This study finds that the change of the total and motor FIM scores in both groups were significantly higher for the patients able to return home in our study. Of the selected motor sub-scores, only the item for intimate hygiene changed significantly during rehabilitation, thus validating our clinical observation that this seems to be a key component for returning home.
Patients with FIM scores <5 for items such as grooming, bathing, dressing and locomotion are still able to return home, even if they live alone, as long as they are independent (FIM ≥6 for each) in motor and cognitive sub-scores such as eating/drinking, intimate hygiene, bladder and bowel management, bed/stool/wheelchair/toilet transfer, acoustic/visual understanding, verbal/nonverbal expression, social behavior, and problem solving.
Although age might be expected to have an influence on discharge accommodation, it was not an independent risk factor in this study. Our interpretation is that age has less of an influence on patient functionality than multimorbidity. Whether the underlying medical condition is a significant predictor of discharge destination is uncertain.13,17 Another observation, again not unexpected and found by others,17 was that patients discharged to an institution had longer length of stay. We interpret this finding as a consequence of our early discharge planning. If the general disposition of a patient is weak and discharge to home is therefore uncertain, we plan for both outcomes very early on during the rehabilitation and organize applications for the entry into a nursing home with the patient and the family. Sometimes these patients will remain in rehabilitation for longer periods of time in the hope that an entry into a nursing home can be prevented.
A previous study6 found that a cut-off value of ≥78 (total FIM score) satisfactorily predicted the location of discharge. This score correctly classified more than 75% of patients discharged to the community and institutional settings (FIM score ≤78) respectively. In our sample this value provides good sensitivity (74.4%), but poor specificity (37.0%). Yet it correctly determined the discharge location of 80.2% of patients. Hence approximately 20% of patients with a total FIM score <78 where discharged home, or discharged to an institution with a score >78. This shows that in practice the total FIM score is not a reliable predictor of discharge destination. In our experience the destination is determined by extensive discharge planning according to the goal settings defined by the International Classification of Functioning, Disability and Health within the patient’s individual resources, context factors and the individual FIM scores, especially the sub-scores for intimate hygiene, bladder and bowel management. The fact that divorced patients showed highest FIM may reflect a strong resolve by these patients to be autonomous.
LIMITATIONS
A limitation of the study is that the use of marital status as a proxy for living with someone may lead to some misclassifications – some married patients may live alone for some reason, while some unmarried, divorced or widowed patients may live with a caregiver e.g. children, or other partner. This information is not gathered in our hospital administrative database.
In addition, the exclusion of a third of all patients presenting to our service due to defined criteria and incomplete data sets may have produced a study group with unexpectedly good functionality as seen with the high admission FIM grade.
CONCLUSION
In this study, age was positively related to institutional discharge. All FIM scores – total, motor and cognitive, were positively related to the probability of discharge home. Generally, total FIM scores discriminated best between patients discharged to a nursing home or their own home but that score alone is not able to predict accurately discharge location. Discharge planning is an essential part of the rehabilitation process, influenced by several context factors and resources inherent to the patient and his surroundings. Nevertheless, the practical use of the FIM score requires further study.
Provenance: Externally reviewed.
Ethics: Approval received from the Swiss Ethics Committee, Lausanne.
Disclosures: No disclosures.
Corresponding Author: Dr Wolfram Weinrebe, Department of General Internal Medicine and Geriatric Medicine, Campus Spital Hirslanden, Schänzlistrasse 39, 3032 Bern, Switzerland.
Email: wolfram.weinrebe@hirslanden.ch









